What is TMS Therapy?
TMS Therapy or Transcranial Magnetic Stimulation treatment is a safe, non-invasive treatment of depression that has been approved by Health Canada in 2002 and the FDA in 2009. It is a safe treatment where 65-70% of patients suffering from treatment-resistant depression get considerable relief and 50% become completely symptom-free. In other words, even after other treatments have failed to help someone with depression, TMS Therapy can improve most people who suffer from a stubborn depression, but not all. It is non-invasive and has very little side-effects. It is well-tolerated by the majority of people. There are two significant technologies currently available in Canada, regular rTMS and Deep TMS and we offer both. TMS Therapy is not currently covered by OHIP but Health Quality Ontario has submitted a report recommending that it be covered as soon as possible

How does TMS work?
Do you remember electromagnetic fields?
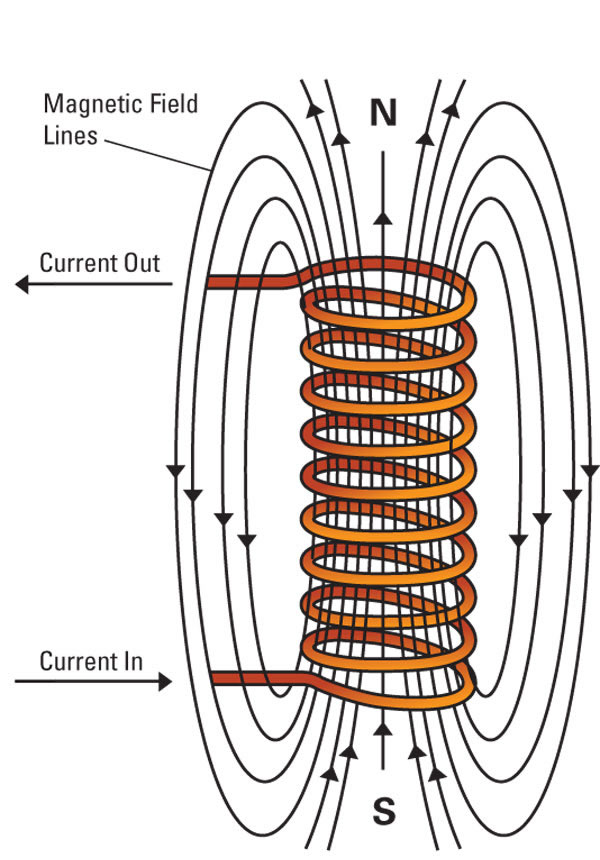
If you recall science experiments in school, you might remember experiments where you wrapped copper wire around a metal bar or a nail. And this turned the bar into an electromagnet and you were able to pick metallic things up with it. TMS Therapy uses a very sophisticated and powerful electromagnetic coil. A specialized computer controls the intensity and parameters of the treatments.
The coil is operated at a given frequency where it is activated then turned off many times a second. This pulsating electromagnetic field goes through the skin and skull easily and interacts directly with the neurons in the brain. This pulse can either stimulate or inhibit the neurons, depending on the frequency of the pulse.
Contrary to popular belief, the brain is able to change and adapt. After years of research, it is now very clear that the brain is capable of changing, something we call neuromodulation. Electromagnetic stimulation of the brain, with a pulsing electromagnetic field, is one of the many ways to effect neuromodulation.
In TMS Therapy, the pulsing electromagnetic field causes the release of neurotransmitters and nerve growth factors. TMS also causes an increase in blood flow to that area. The connections between neurons, called synapses, increase in density after a series of treatments. The area stimulated reconnects to other areas in the brain, that are nearby and can even reconnect with areas at a distance.
TMS Treatment of Depression
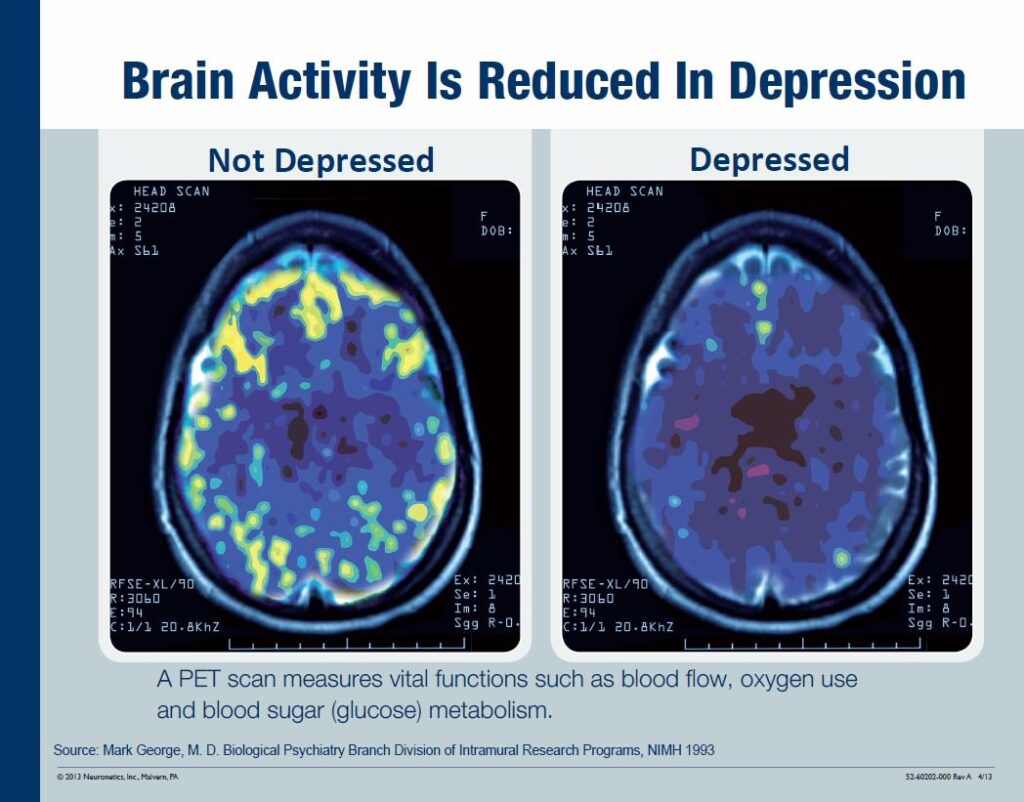
In depression, a PET Scan of the brain shows that the dorsolateral prefrontal cortex (DLPFC) is underactive. The DLPFC connects and influences the limbic system, the complex circuit in the brain that is associated with mood and emotions. Therefore, the DLPFC influences our moods, indirectly. The underactive DLPFC connection to the limbic system is not as strong in depressed people. The DLPFC becomes active again after TMS Therapy, as shown by a repeat PET Scan. And this correlates with improvements in depression.
TMS Therapy for other ailments
Other conditions such as anxiety, Obsessive-Compulsive Disorder, Post-Traumatic Stress Disorder and Traumatic Brain Injury can also be treated.
Who can benefit from TMS Therapy?
Health Canada and the FDA approve TMS Therapy in the treatment of treatment-resistant Major Depressive episodes. TMS Therapy is a first-line treatment for treatment-resistant depression as per the 2016 CANMAT guidelines.
Not everyone benefits
Every person is different and as such, results will differ from person to person. TMS therapy may be able to alleviate your symptoms of depression or help them disappear entirely. Typically, relieving depressive disorder symptoms may take several weeks of treatment.
Is TMS therapy safe?
Although long-term effects of exposure to TMS Therapy are not known, there are no significant short-term or long-term safety concerns associated with exposure to other devices such as MRI scanners. Therefore, it is unlikely that there are any long-term effects to getting TMS Therapy.
Side-effects of TMS Therapy
TMS Therapy does not have the side-effects of antidepressants. Some patients report fatigue in the hours after a treatment. TMS Therapy can cause headaches and scalp discomfort. TMS Therapy is well-tolerated and the risks of adverse events are minimal.
Common Side-Effects
- Headache
- Scalp discomfort at the site of stimulation
- Tingling, spasms or twitching of facial muscles
- Lightheadedness
- Discomfort from noise during treatment
- Changes in energy levels (increase or decrease)
- Teary eye(s)
Very Rare Side-Effects
- Seizures (about a 4/50,000 chance)
- Hearing problems
- Hypomania/mania
- Exacerbation of depressive symptoms
- Nightmares/Vivid Dreams
What do I do if I’m interested in TMS Therapy?
If you or your healthcare provider has determined that TMS Therapy may be right for you, Book a Consultation Now with our Registered Nurse.
Free assessment
During this assessment, we will screen for contraindications to TMS Therapy, as well as discuss your medical and psychiatric history and medications. The initial assessment acts to ensure that you are a suitable candidate for TMS Therapy. Any of your remaining questions or concerns can be raised at this time. Intake forms and a new patient informational packet will be provided.
What happens during the treatment?
Treatment is administered by a trained technician and overseen by a medical doctor. You will get a chance to familiarize yourself with the equipment and treatment procedure prior to starting the first session. During treatment, patients are fully conscious and able to read, listen to music, or talk with the provider. TMS therapy is an outpatient procedure which means that no hospitalization is required. The TMS therapy procedure itself is non-invasive and requires no anaesthesia.
First Day of TMS Treatment
The intensity of the electromagnetic field that will be delivered is determined by stimulating the area of your brain responsible for contracting your thumb muscle and thereby making your thumb move. That’s called “Determining your Motor Threshold (MT)”. It allows us to actually see how much electromagnetic energy is needed to depolarize your neurons and this amount of energy is called the MT. You may feel a tingling or tapping sensation on the head. Scalp muscles may feel a little tense, during and a bit after the procedure. This is normal and may result in a minor headache. There may be some pain in the first 3 sessions so we stimulate at a slightly lower intensity so you can get used to it. Then we continue at the determined intensity.
Duration of TMS Treatment
TMS treatment of depression is divided into 3 phases:
Phase 1 – The Acute Phase
In the Acute Phase, we aim to give you the maximum improvement of your depression. On average, patients require between 30 and 50 daily treatments, 5 days a week, for this phase. The actual number of treatments depends on the severity and duration of your illness and any complication. Factors that can complicate your illness are such things as having other diagnoses.
Phase 2 – The Stabilization Phase
The Stabilization Phase immediately follows and its goal is to maintain the gains you have achieved in the Acute Phase. The stabilization phase prevents the reappearance of the symptoms of the current episode. This phase consists of 1-3 treatments a week for 8-12 weeks.
Phase 3 – The Maintenance Phase
The third phase is the Maintenance Phase and will follow the second phase for some people. Not everyone needs the maintenance phase. The Maintenance Phase can be with medication alone or can include both TMS treatments and medication. This phase’s goal is to prevent a recurrence or a new episode over time. Many things factor into the decision to do maintenance. Some people will need maintenance for 3-5 years and others will need it for life. If you choose to have Maintenance TMS Therapy, you should get 1-2 treatments every 3-6 weeks.
Communication with Staff
It is important that you feel comfortable at HeadWay Clinic. Please feel free to discuss any concerns that you have, and to ask questions as they may arise. HeadWay Clinic staff members appreciate learning how we can help make your treatment experience as pleasant as possible. Of course, you can stop TMS Therapy anytime you want.
Your last day of treatment
We use clinical scales and verbal report from the patient to determine the response to the treatment. At the end of the treatment, our medical staff will review with you your treatment and discuss ongoing needs and answer any outstanding questions.
Follow-Up
Our team wants to keep in touch with you after your treatments are finished.
- We encourage regular follow-ups by phone or email.
- We encourage you to call with your questions.
FAQ
No, it’s not yet covered by OHIP. In 2016 Health Quality Ontario (HQO) submitted a report to the Ministry of Health and Long Term Care and it recommended that TMS Therapy be a covered benefit of OHIP but the ministry never did anything with it. Recently, MOHLTC requested an updated report from HQO and Dr Gagnon was part of the expert panel advising them. We are hopeful that TMS will be covered in the next couple of years but we don’t know for sure.
Please contact your benefit or insurance provider to see if you qualify for full or partial coverage of TMS therapy. If you were involved in a motor vehicle accident, your insurance will likely cover it if it is necessary and reasonable. Blue Cross for Veterans Affairs and active Canadian Forces personnel will usually cover it for PTSD and Depression.
Yes, it is!
You can’t have any ferrous metal in your head or your eyes to be eligible for TMS. A titanium aneurysm clip is fine as it isn’t subject to magnetic forces. You can’t have a cochlear implant or pacemaker. In other words, if you can have an MRI, you can get TMS. If you suffer from a seizure disorder, you should not get TMS. For further information contact any one of our sites to get screened or if you have any questions.
Many patients are able to stop their antidepressants once they respond to TMS Therapy. Some prefer to stay on them as the two therapies act synergistically to help relieve depressive symptoms. Also, studies have shown that TMS treatments can “revive” an antidepressant that had lost most, if not all, its beneficial effects on a patient. That antidepressant can also be used to do the Maintenance Therapy if continuing with periodic TMS treatments is not possible.
TMS therapy is not at all like Electro Convulsive Therapy (ECT). ECT is a treatment based on using electricity to induce seizures. It is very effective and in many cases, it is a life-saver. ECT requires anesthesia and can have serious side-effects, including memory loss. It is only done in a hospital. On the other hand, Transcranial Magnetic Stimulation uses magnetic pulses to non-invasively stimulate specific brain regions associated with major depressive disorder. No seizures are required for the treatment to be effective, and they are a very rare adverse event (< 4/50000) that we avoid at all costs. TMS therapy is performed in our office, requires no anesthesia, and has no systemic side effects.